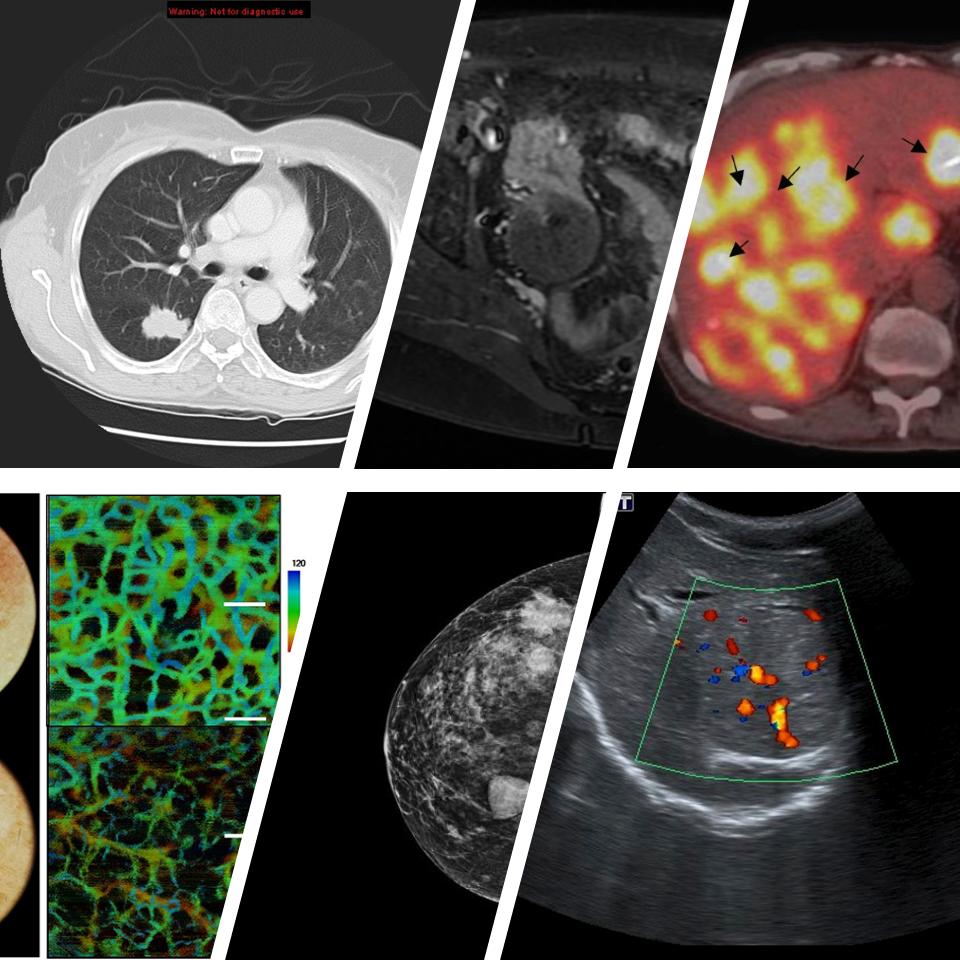
Uses of Imaging
Imaging, by itself, is not a treatment, but it is a tool that can help in making better decisions about treatments. The same imaging technique can help doctors find cancer, tell how far a cancer has spread, guide delivery of specific treatments, or find out if a treatment is working. Imaging can be used for the following purposes:
- Screening for cancer: Imaging can be used to determine if a person has any suspicious areas or abnormalities that might be cancerous. Mammograms are an example of a familiar imaging tool used to screen for breast cancer. Screening for cancer is usually recommended for people who are at increased risk (due to their family history, lifestyle, or age) for developing a particular type of cancer.
- Diagnosis and staging: Imaging can be used to find out where a cancer is located in the body, if it has spread, and how much is present. Used in this way, imaging can help determine how advanced the cancer is, and if the cancer is in, around, or near important organs and blood vessels. If a biopsy (taking a small amount of the tumor for laboratory examination) is necessary, imaging may be used to help guide doctors to the tumor and take a sample of it.
- Guiding cancer treatments: Imaging can help guide delivery of cancer treatments. Imaging can be used to make cancer treatments less invasive by narrowly focusing treatments on the tumors. For instance, ultrasound, MRI, or CT scans may be used to determine exact tumor locations so that therapy procedures can be focused on the tumor, minimizing damage to surrounding tissue.
- Determining if a treatment is effective: Imaging can be used to see if a tumor is shrinking, or if the tumor has changed and is using less of the body's resources than before treatment.
- Monitoring for cancer recurrence: Imaging can be used to see if a previously treated cancer has returned or if the cancer is spreading to other locations.
Radiation Risk
Sometimes patients get frightened by the word "nuclear", but doctors have been using nuclear material for medical uses since before World War II.
Your doctors are concerned about keeping your exposure to radiation as low as possible. Some tests, such as diagnostic MRI and diagnostic ultrasound do not have any radiation that might hurt you. Other common tests like x-rays have a very small radiation dose, equivalent to other everyday activities such as driving a few miles. Other tests, such as CT scans, PET, or nuclear medicine exams have higher radiation doses, but doctors order these when medically necessary. Some examples of when these might be medically necessary are:
- When the results of imaging might change your diagnosis or treatment
- When the benefits of having more precise imaging to guide treatment exceeds the small risks posed by radiation exposure
- When imaging is less risky and invasive than other methods of obtaining the same information, such as exploratory surgery
Medical professionals take extra safety precautions with pregnant women and children. Imaging professionals are also sensitive to the fears that children and other people may have of the equipment and will try to ease your anxiety about the procedure.
X-Ray Imaging
X-ray imaging is perhaps the most familiar type of imaging. X-rays use the different absorption rates of different tissues to produce images. Calcium in bones absorbs x-rays the most, so bones look white on a film recording of the x-ray image, called a radiograph. Fat and other soft tissues absorb less and look gray. Air absorbs least, so lungs look black on a radiograph.
The most familiar use of x-rays is checking for broken bones, but we can also use x-rays to look for or diagnose cancer. For example, chest radiographs and mammograms are often used for early cancer detection or to see if cancer has spread to the lungs or other areas in the chest.
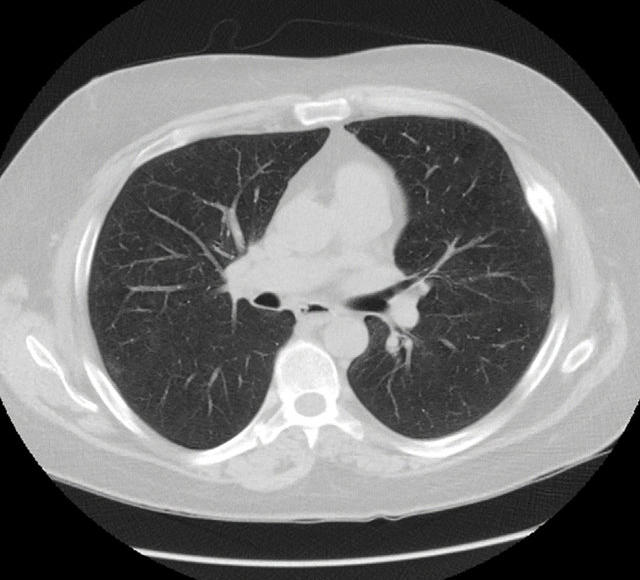
CT Scans
A computed tomography scan (CT scan, also called a CAT scan) uses computer-controlled x-rays to create images of the body. However, a radiograph and a CT scan show different types of information. Although an experienced radiologist can get a sense for the approximate three-dimensional location of a tumor from a radiograph, in general, a plain radiograph is two-dimensional.
An arm or chest radiograph looks all the way through a body without being able to tell how deep anything is. A CT scan is three-dimensional. By imaging and looking at several three-dimensional slices of a body (like slices of bread) a doctor can not only tell if a tumor is present, but roughly how deep it is in the body. A CT scan can be three dimensional because the information about how much of the x-rays are passing through a body is collected not just on a flat piece of film, but on a computer.
The data from a CT scan can be enhanced to be more vivid than a plain radiograph. For both plain radiographs and CT scans, the patient may be given a contrast agent to drink and/or by injection to more clearly show the boundaries between organs or between organs and tumors.
Molecular Imaging (PET and SPECT)
Molecular and nuclear imaging use low doses of radioactive substances linked to compounds used by the body's cells or compounds that attach to tumor cells. Using special detection equipment, the radioactive substances can be traced in the body to see where and when they concentrate.
PET Scan
The positron emission tomography (PET) scan creates computerized images of chemical changes, such as sugar metabolism, that take place in tissue. Typically, the patient is given an injection of a substance that consists of a combination of a sugar and a small amount of radioactively labeled sugar. The radioactive sugar can help in locating a tumor, because cancer cells take up or absorb sugar more avidly than other tissues in the body.
After receiving the radioactive sugar, the patient lies still for about 60 minutes while the radioactively labeled sugar circulates throughout the body. If a tumor is present, the radioactive sugar will accumulate in the tumor. The patient then lies on a table, which gradually moves through the PET scanner incrementally several times during a 15-60-minute period. The PET scanner is used to detect the distribution of the sugar in the tumor and in the body. By the combined matching of a CT scan with PET images, there is an improved capacity to discriminate normal from abnormal tissues. A computer translates this information into the images that are interpreted by a radiologist.
PET scans may play a role in determining whether a mass is cancerous. However, PET scans are more accurate in detecting larger and more aggressive tumors than they are in locating tumors that are smaller than 8 mm (a pinky nail or half of a thumb nail) and/or less aggressive cancers. The size of smallest tumor mass that can be found using PET is constantly improving. They may also detect cancer when other imaging techniques show normal results. PET scans may be helpful in evaluating and staging recurrent disease (cancer that has come back). PET scans are beginning to be also commonly used to check if a treatment is working - if tumor cells are dying and thus using less sugar.
SPECT Scan
Similar to PET, single photon emission computed tomography (SPECT) uses radioactive tracers and a scanner to record data that a computer constructs into two- or three-dimensional images. A small amount of a radioactive drug is injected into a vein and a scanner is used to make detailed images of areas inside the body where the radioactive material is taken up by the cells. SPECT can give information about blood flow to tissues and chemical
reactions (metabolism) in the body.
In this procedure, antibodies (proteins that recognize and stick to tumor cells) can be linked to a radioactive substance. If a tumor is present, the antibodies will stick to it. Then a SPECT scan can be done to detect the radioactive substance and reveal where the tumor is located.
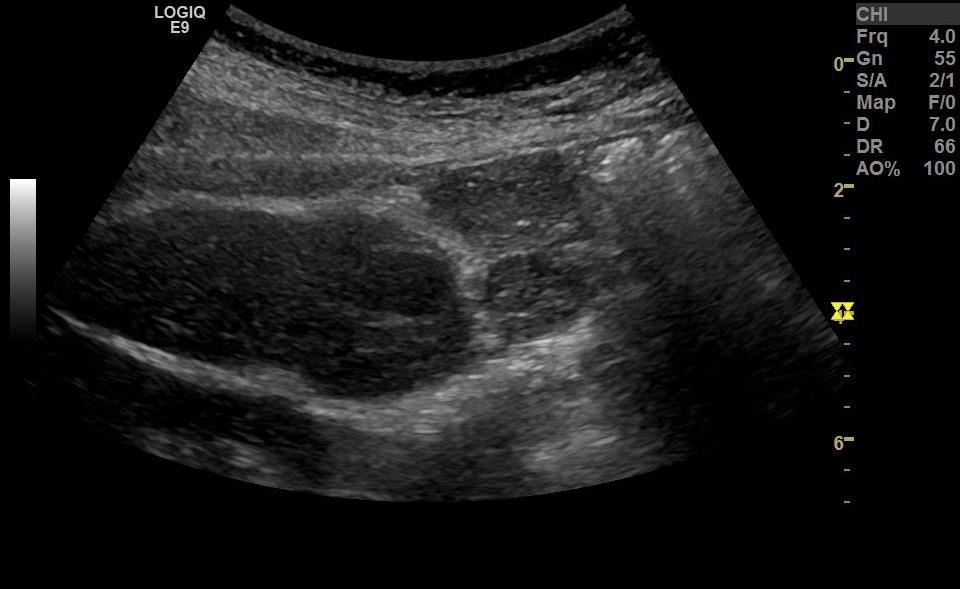
Ultrasound
Ultrasound (US) uses sound waves with frequencies above those humans can hear. A transducer sends sound waves traveling into the body which are reflected back from organs and tissues, allowing a picture to be made of the internal organs. Ultrasound can show tumors and can also guide doctors while they are doing biopsies or treating tumors. Most people know about US images when a woman is pregnant, for example — boy or girl. As with diagnostic MRI, there is no harmful radiation from diagnostic US. (Keep in mind, both MRI and US can be used for treatment under certain conditions - but this very uncommon currently.) Unfortunately, while US is very useful for imaging certain body parts, it is not as useful as other imaging techniques for looking at the brain, lungs, or an entire abdomen or pelvis. Because masses can sometimes be tiny and far from the skin surface, we usually need CT, MRI, and/or PET to find these places of suspect tumor spread.
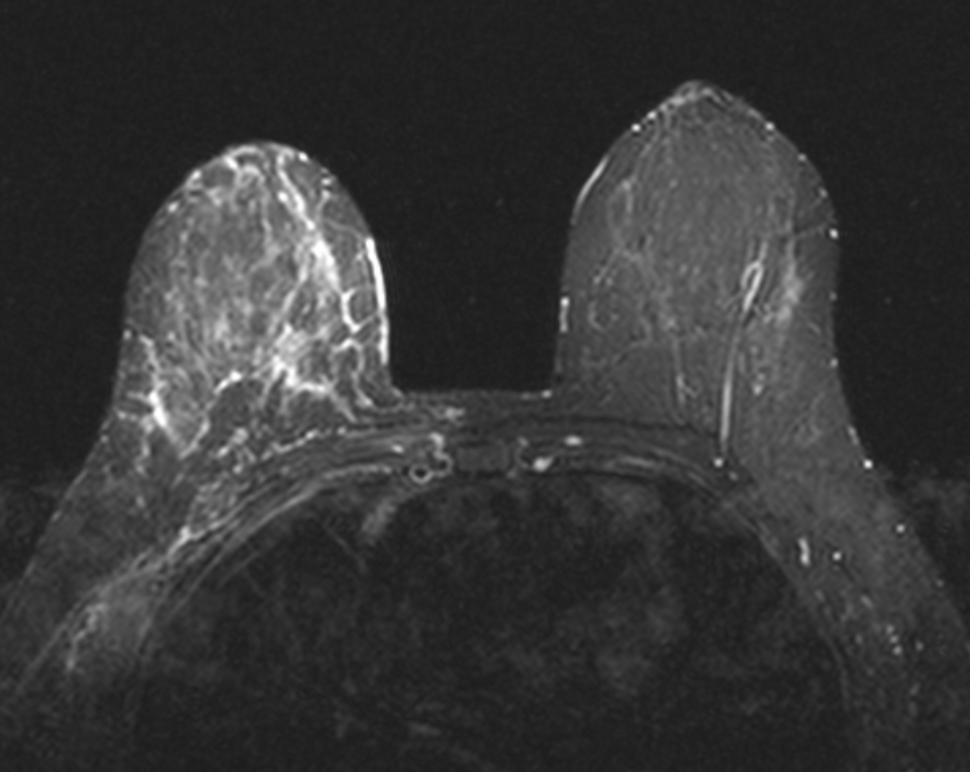
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) uses radio waves in the presence of a strong magnetic field that surrounds the opening of the MRI machine where the patient lies. The radio waves get tissues to emit radio waves of their own.
Different tissues (including tumors) emit a more or less intense signal based on their chemical makeup, so a picture of the body organs can be displayed on a computer screen. Much like CT scans, MRI can produce three-dimensional images of sections of the body, but MRI is sometimes more sensitive than CT scans for distinguishing soft tissues.
Many people know that MR scanners are noisy. Most MR technologists have a big supply of ear plugs or an over-the-ear headphone for the patient to use. Some people get claustrophobic in the MR units. The doctors and technologists are accustomed to helping patients deal with this.
MR is safe — so long as there is no metal in your body.
MR is safe for pregnant women and kids — there is no harmful radiation from MRI.
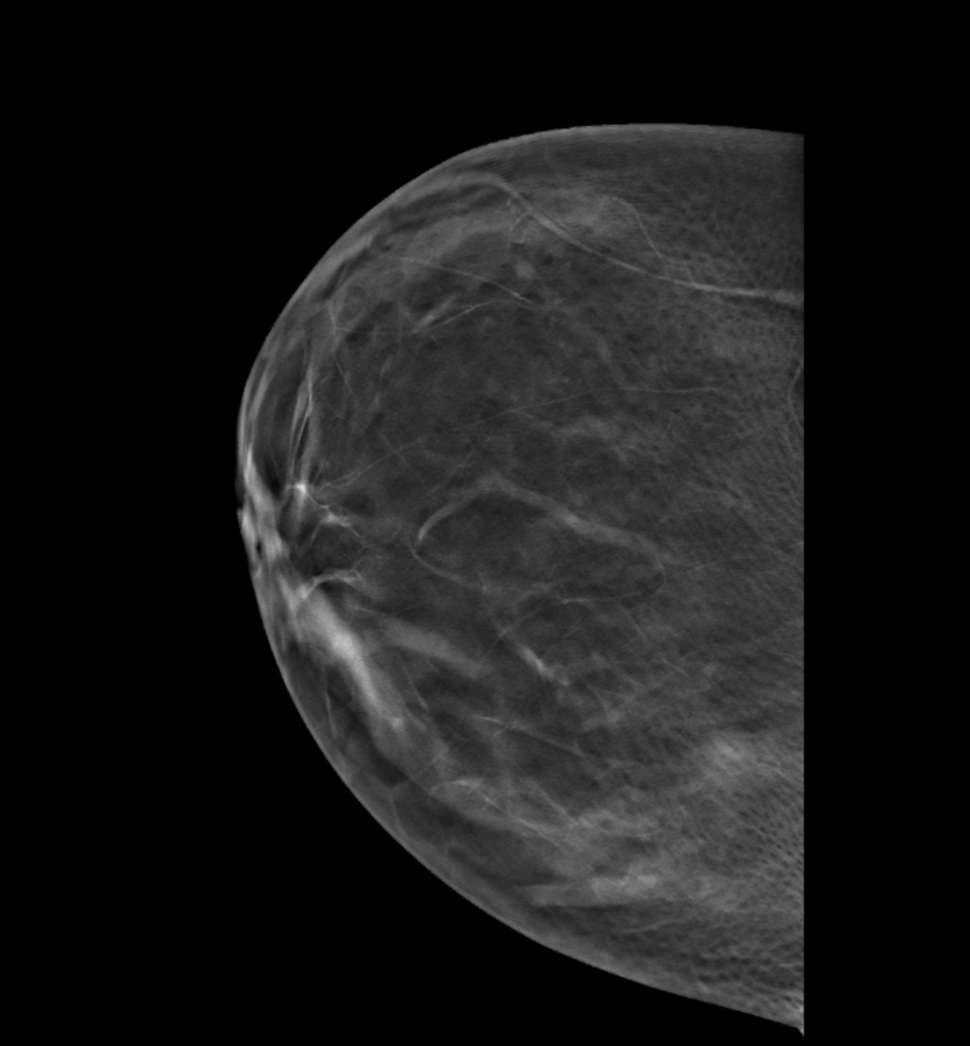
Digital Mammography
Conventional mammography uses x-rays to look for tumors or suspicious areas in the breasts. Digital mammography also uses x-rays, but the data is collected on computer instead of on a piece of film. This means that the image can be computer-enhanced, or areas can be magnified. Eventually, a computer could be used, in certain appropriate situations, to screen digital mammograms, theoretically detecting suspicious areas that human error might miss. There are both 2D and 3D forms of mammography available today.
In addition to "regular" mammograms, additional or spot views might be needed if a suspicious finding is noted on a screening mammogram (meaning no tumor was suspected by history nor by physical exam when the test was ordered).
US and MRI are other types of diagnostic tests that might be obtained to assess the breast.
Sometimes a biopsy is recommended in order to get a piece of tissue for the pathologist to examine. This will determine if a tumor might be present.
In most every part of the body except for the breast, most biopsies find cancer or something else bad. In the breast, 80-90% of biopsies do not show any tumor. However, because imaging findings for cancer and non-cancerous abnormalities are similar, we have not yet found a way to improve on this low yield.
Breast cancer also occurs in men. So a man with a new chest mass should also see his doctor.
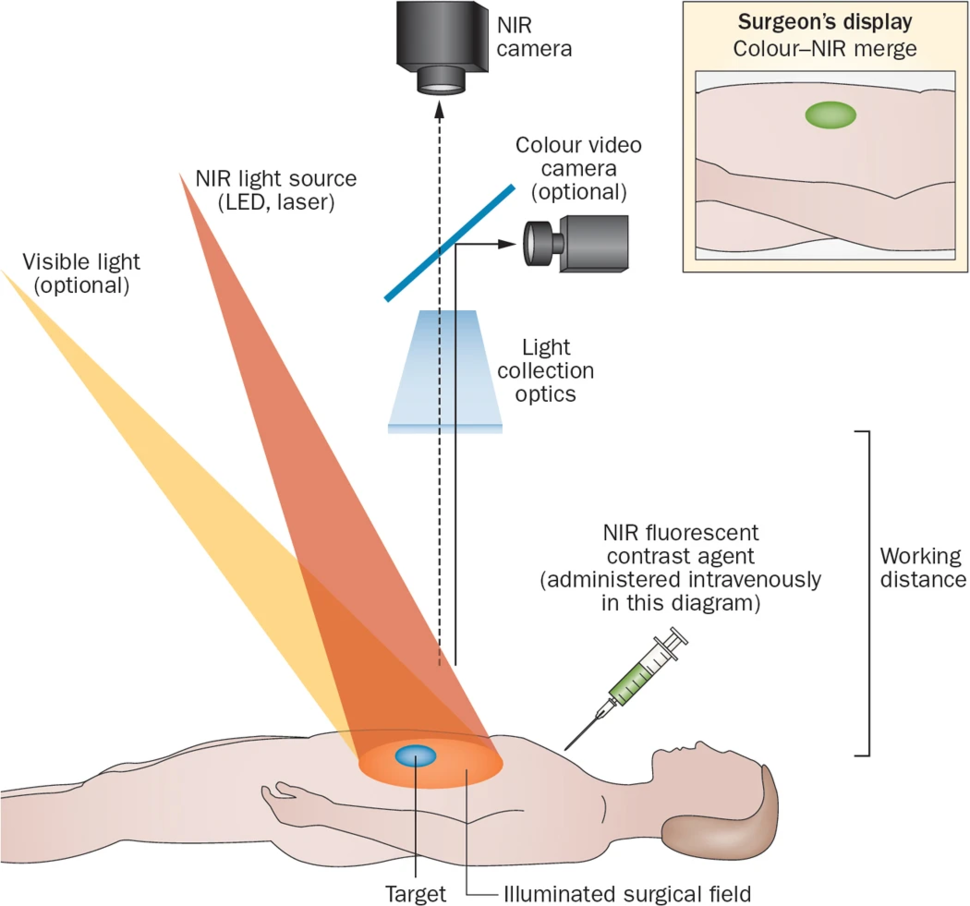
Sentinel Node Mapping
This technique illustrates how imaging may be able to reduce the need for extensive diagnostic surgery. When patients are being diagnosed with breast cancer it has been standard practice to surgically remove all of the lymph nodes under the arm to determine if the cancer has spread beyond the breast and what treatment is appropriate. Removing all the lymph nodes can result in long-term complications and discomfort for the patient from bad arm swelling called lymphedema (a condition where excess lymph fluid collects in tissues and causes swelling). Trials are underway now, however, to test an alternative, less damaging procedure in which imaging plays an important role.
In this alternative procedure, called sentinel node mapping, only the sentinel node (the first lymph node to which breast cancer is likely to spread) is removed rather than all the lymph nodes. In order to identify the sentinel node, the doctors inject either a blue dye or a relatively non-toxic radioactive substance and see which lymph node it reaches first. This lymph node is the sentinel node, and is surgically removed.
This has been done since the 1990s at many centers. It is becoming more common for assessment of breast tumor spread.
Image-Guided Surgery
Image guided surgery is most commonly used by brain surgeons. When you hear about a brain surgery patient having a big metal or plastic frame around their head, this is part of the localization system.
Various techniques for this have been around since the 1990s. These systems fuse imaging data from a pre-surgical CT or MRI to location information which can be used by the surgeon during the neuro-surgical procedure. This can make the procedure both faster and safer.
There are multiple techniques for using imaging to guide surgery in the body, for example in the liver. This is an area where technique changes occur often.